When the hip joint is quite worn, and other measures have failed to improve pain or restore your quality of life, surgery may be an option. Hip Replacement Surgery also called Arthroplasty, has been commonplace since the 1960s and represents one of the significant achievements in healthcare in the 20th century.
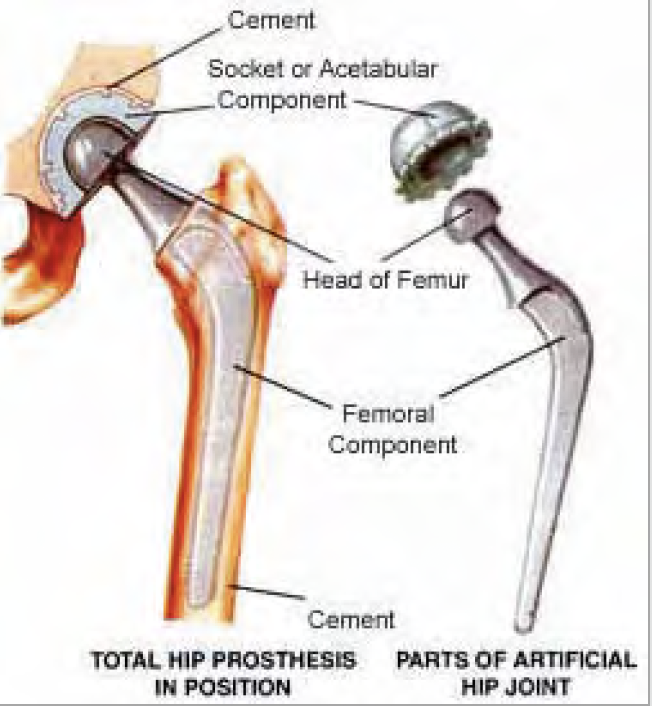
A Total Hip Replacement involves the removal of a painful Hip Joint and replacing it with a new ball and socket into the arthritic hip joint, helping relieve hip pain and resume mobility. The procedure is usually conducted under a spinal anaesthetic, but it can be combined with some sedation so that you are effectively asleep.
Your Hip Surgeon makes an incision over the side of the hip bone, and the joint is accessed by releasing a small portion of the muscles around the painful joint.
Once the joint capsule has been opened, the hip is popped out of the socket, and the worn head of the femur is removed. The acetabulum or socket is then prepared with special instruments that scrape off any remaining cartilage. The new cup is inserted, and this can be either pressed in, secured with screws or cemented in place. The space down the femur bone is then enlarged to accept the new femoral component, and it can also be pressed in or cemented into place. The new head fits on to the femoral component, and the hip is reduced back into the socket. Final checks for length and stability are made, and any muscles that were released are then repaired, and the wound is closed.
Patients are usually genuinely quite surprised at how quickly they begin to recover following a hip replacement. This may well mean taking your first few steps the day of the operation!
Crutches are used for most activities for approximately six weeks, depending on surgeon preference, but these are mainly to help with balance and minimise the risk of a fall.
During your hospital stay (usually 2 to 4 days after your surgery) at UPMC Sports Surgery Clinic, our physiotherapy team supervises your exercises and mobilisation until you are independently mobile.
| For further information on Total Hip Replacement Surgery or to make an appointment please contact infossc@upmc.ie |
There are many common conditions which require a hip replacement as the treatment. For example the most common is osteoarthritis. Osteoarthritis simply means that the cartilage of the hip has worn out resulting in the thighbone and pelvic bone rubbing together. As you know this is very painful and stops you being able to move your hips as you once did.
All patients scheduled for joint surgery must attend the Pre-Assessment Clinic (PAC) following referral by their consultant and are invited to attend 3-4 weeks before proposed surgery. This ensures that all tests results are valid for admission and allow time to resolve problems if identified during PAC, so surgery can be performed without delaying the planned surgery date. The PAC is a comprehensive medical assessment taking place to ensure patients are fit for surgery, therefore minimising risk and ensuring a speedy recovery. While avoiding cancellation and disappointment on the day. At the clinic you will be seen by a nurse and a doctor To make sure you are fit for the operation and anesthetic a number of tests will be carried out, they will include the following:
- Electrocardiogram (ECG) which is a non – invasive heart investigation which takes couple of minutes to perform.
- Blood pressure and heart rate.
- Urine sample to test for urinary tract infection (UTI) and diabetes.
- Methicillin Resistant Staphylococcus Aureus (MRSA) screening this includes swabs from nose and groin. This is a bacteria resistant to some antibiotics.
- Blood tests.
- Blood type and screen this is done in case we need to give a blood transfusion during or after your operation.
- Body mass index (BMI).
- lDetailed patient history.
- lExamination by medical doctor.
Please ensure that you bring the following with you on the day of PAC
- All medication in the original labelled containers, that you are currently taking. It is important that the medication is not repackaged into a weekly pill dispenser/pill box.
- Relevant x-rays, MRI, CT including any chest x-rays taken within the last three months or relevant joint
- x-rays taken within the last six months.
- Please bring the address and phone number of your GP and any other consultant or specialist you are currently attending.
- Please bring any results or reports from any past ECG, ECHO or angiograms.
- Please ensure that your first name and date of birth is as it appears on your birth certificate.
- Please ensure that the pre-operative questionnaire is completed.
- The whole PAC visit will approximately take one hour.
Before your surgery it is important to maintain an active lifestyle so that the muscles around your hip stay strong. Research has shown that patients who do an exercise program pre operatively have a quicker recovery than those who don’t.
Knowing what to expect, practicing drills on early post-op management and exercising before your surgery will help you to increase your confidence and ability to exercise after your operation.
At SSC we run weekly prehabilitation classes in our physiotherapy department gym. This class consists of an education section where you learn about your surgery and what to expect. We also give you exercises to help you prepare for your surgery, and practice using crutches so you can be confident after your surgery and during your rehabilitation. We explain in detail what you can expect from physiotherapy after your operation and give you some practical tips. We will answer any questions or concerns you have about your rehabilitation.
To book your class please contact the SSC physiotherapy department on 01-5262040.
You will be admitted into SSC either the day before or morning of your operation.
On admission, you will check in at the reception area and be asked to confirm your details for your medical file. A member of the admissions staff will accompany you to the Inpatient Ward where you will be greeted by the nursing staff. The nursing staff will show you to your bed and will check your weight, height, temperature, blood pressure, pulse and respiratory rate. The nursing staff will also update and complete the nursing assessment that was started in PAC. You will also see other members of the treating team at this time. If you have any questions do not hesitate to ask a member of staff.
- If you take medication on a regular basis please bring this with you, in its original packaging, as we may use this when you are in SSC.
- Please remember to remove false nails/long term nail varnish before coming into SSC.
- We advise that you bring nightwear, a dressing gown, slippers (flat, closed heel slippers) or walking shoes, reading glasses and toiletries. You will also need some day wear for your discharge from the clinic.
- We advise that you do not bring valuables into hospital with you. You may keep your wedding ring on (which will be covered with tape) when you go to theatre but this is the only jewellery that you will be allowed.
- The doctor will draw an arrow on your hip to indicate which one is being operated on.
- You cannot eat or drink anything for at least 4 hours before your operation, so you will usually be ‘Nil By Mouth’ from 12midnight (for a morning operation) or 6a.m. (for an afternoon operation). The nursing staff will remind you about this. This includes chewing gum.
- On the morning of your surgery you will be given a theatre gown to change into. You will be asked to remove make up, nail polish and jewellery apart from a wedding band, which can be taped over.
- You will be wearing one white stocking, which is called a TED stocking, on the opposite leg i.e. the leg you are not having your operation on. The stocking
- is applied to help improve the circulation in your
- legs and so reduce the risk of getting a blood clot. A stocking will be applied to your operated leg after your operation.
- The anaesthetist , who is the doctor that will be administering your anaesthetic, will talk to you before your operation. He / she will talk to you about your general health and any previous anaesthetics. He/she will check your lab tests and all other relevant tests and letters from other specialists. They will then advise you of the safest anaesthetic for you with regard to the operation you are having done.
For total hip/knee replacements:
Spinal anaesthetics are the most commonly used anaesthetic. An injection is carefully placed in the lower back area, this causes your legs to become numb. They stay numb all the way through the surgery and come back to normal later. While you are in the operating theatre your Anaesthetist will give you other medication, which will relax and sedate you. You are very unlikely to hear or see any part of the surgery. General Anaesthetics are rarely used for joint replacement surgery. However if your anaesthetist recommends that you have a general anaesthetic, you will receive medication via the intravenous cannula in your hand/arm, then you will drift off to sleep and wake up in the recovery room when the surgery is completed.
- You will be taken to theatre on your bed. A nurse
- will accompany you to theatre. In the reception area the theatre staff will check your details and ask you several questions such as when you last ate or drank and which hip is being operated on. This is all quite normal, as we like to check these details several times.
- From the reception area you will be wheeled into
- the anaesthetic room where you will have your anaesthetic. Once you have had your anaesthetic you will be transferred into the operating theatre.
- The operation usually takes 1 hour to do but you will be off the ward for longer than this because you will need time to have the anaesthetic before the operation and to recover after the operation.
- You will be wheeled from the operating theatre into the recovery room where you will be closely monitored by the nursing staff. The nurses will check that you are recovering from your anaesthetic by checking your blood pressure, pulse, breathing rate and so on. Once they have assessed that you are recovered enough you will be transferred back to the ward on your bed.
- lYou will have oxygen delivered either through a mask over your nose and mouth or through a small double pronged tube which sits at the nasal passages and you will have a bag of fluid running through a tube into one of your veins.
- You may be attached to a pain pump. This pump is called a Patient Controlled Analgesia (PCA) pump. The PCA delivers a small amount of painkiller called morphine into your bloodstream when you press button on the handset. You cannot overdose yourself, as there is a lock out device on the machine. This means that you can press the button on the handset many times but you will only get the one dose that is due within the timeframe. The PCA can make you feel dizzy or sick Please let the nurses know if you have any side effects.
- lThere may be a drain placed on one side of your wound to drain any excess blood or fluid from your wound that could cause delayed healing of the wound. The excess blood/fluid is drained into a collection bottle attached to the drain.
- lYou will have a large triangular shaped foam wedge between your legs, at knee level, which is called an abduction wedge. This is in place to stop you crossing your legs. This will be kept in place for several days whilst you are in SSC. The reason you must not cross your legs is because it can cause the hip replacement to dislocate.
- l Once you are back on the ward the nurses will continue to monitor you. You will have your blood pressure, pulse etc checked regularly and your hip dressing will also be checked.
- You will start taking sips of water as soon as you come back to the ward and gradually you will be allowed to eat and drink as you would normally. Many people feel sick after surgery and this can be due to the anaesthetic and medication that you were given during the operation. Once you are eating and drinking again the drip will be taken away. This is usually about 24 hours after the operation.
- If you need to pass urine or have your bowels opened then the nursing staff will assist you in using a bedpan, as you will not be able to walk to the bathroom just yet.
Dislocation means that the metal ball slips out of the plastic socket. In the first six weeks after the surgery, the ball is only held in the socket by muscle tension. During this time, before scar tissue forms around the ball, and before muscle strength returns, the hip is more likely to dislocate. Dislocation occurs in less than 4% (less than 4 in a hundred) of cases, and the hip needs to be put back in place under anaesthetic.
The length of time you will remain in hospital depends on how quickly you recover. This section outlines the stages you have to complete before you go home. Most people achieve these stages within 2-5 days of having the operation.
Stage 1 (the first day after your operation)
- The nursing staff will help you to have a wash in bed, as you will not have been out of bed yet.
- lThe physiotherapist, who will aim to get you up out of bed, sitting in a chair and taking several steps with crutches, will visit you. The physiotherapist will remind you of the exercises to do.
- l The nursing staff will assess whether you need to continue using the PCA. If you do not need to use the machine then it will be removed. You will be given painkilling tablets whilst you are on the PCA and after it is removed we advise that you take these tablets so that you can do your exercises and start walking.
- If present, the drain will be removed from your hip.
Stage 2
- The physiotherapist will continue to assess how you are doing and help you to progress with your exercises and mobility.
- lY ou will have a blood sample taken to check that you have not lost too much blood during the operation.
- If you have not had an x-ray in the recovery room then you will have an x-ray taken of your hip in the x-ray department. A member of staff will take you to the
- x-ray department.
Stage 3
- You will be walking with crutches under guidance from the physiotherapist.
- Your prescription will be arranged by the doctor.
- The physiotherapist will practice the stairs with you.
- T ransport arrangements will be finalised. You will be asked to arrange for a relative or friend to collect you by car.
Stage 4
- You will be discharged home. The nursing staff will go through with you the prescription that you can fill at any pharmacy. If you have any questions about your medicines then please ask the nurses who will be able to help you. Do not forget to take your walking aids with you.
- You will be sent an appointment by your consultants secretary with the date of your follow-up outpatient appointment on it, usually for 6-8 weeks after you go home.
Please note that prescriptions cannot be filled from the pharmacy in SSC.
You will be seen by a physiotherapist from the first day after your operation who will:
- help you with bed transfers
- teach you how to walk with crutches (or a zimmer frame in some cases)
- guide you through an exercise program
- practice stairs with you
You will be allowed to sit out on a chair if you can tolerate it on the day after the operation.
You will be able to get up and walk from the first day
after the operation and generally can put as much weight down through the operative limb as is comfortable (unless otherwise advised by your surgeon).
You will be required to use two elbow crutches. This is to avoid too much pressure on the hip. You will be required to climb the stairs with crutches before being discharged from hospital.
The physiotherapist will work with you in hospital until you are comfortable transferring to and from a bed and chair, are confident performing your home exercises, can mobilise safely with your crutches on the flat and on stairs. It is important to continue your exercise program regularly, as directed by your physiotherapist, on a regular basis after your operation.
In order to progress with your rehabilitation we recommend that you organise an appointment with a Chartered Physiotherapist in an out-patient setting within about two weeks of your discharge from hospital. You can attend SSC for physiotherapy or can make an appointment with a physiotherapist in your area. On discharge from SSC you will receive a referral letter and rehabilitation protocol to give to your out-patient physiotherapist. This will inform the physiotherapist of your surgery and give guidelines for your short and long-term rehabilitation. It is likely that you will need follow up physiotherapy for several months after your operation.
The majority of patients who have hip replacement surgery go home from SSC however some patients feel that they need further care in convalescence.
If you feel that you need convalescence following your hip replacement you will need to arrange this yourself with a private rehabilitation unit before coming into SSC.
- Painkillers and reduced mobility can make you constipated therefore it is important that you drink fluids while in hospital and when you get home. The recommended amount to drink daily is 2 litres, which is about 8 glasses. Water is one of the best things that you can take. The nursing staff can give you some mild laxatives if you need them whilst you are in hospital and you may also be prescribed some to take home with you.
- W e advise that you keep the TED stockings on for 6 weeks after your operation provided that you have someone at home to help you take them off at least once a week. The reason for this is so that you can wash and moisturise your legs, as the stockings tend to dry the skin on your legs quite quickly.
- If you have staples or stitches in your hip wound these will be will be removed from your wound between 10-12 days after your operation. You can either attend the wound clinic in SSC or your GP for this.
- It is normal for your leg/hip to be quite bruised after the operation. This will fade in time.
- You should not drive for a period of time after your operation and this will be discussed when you come to the outpatient clinic. You can travel in a car as a passenger from the time you leave hospital.
- You should not fly for approximately 3 months after your operation, as you are at increased risk of a blood clot in your leg veins.
- The leg takes time to adapt to the hip replacement and it is quite common to experience discomfort around the hip for up to 6 months after the surgery. This is not as painful as the arthritis you had and is usually relieved by rest or a mild painkiller. Some patients describe a feeling of tightness around the hip, which usually goes away after a few months but which can return at times. Some patients are left with an area of numbness around the hip, where the nerves, which are cut during the operation, do not rejoin. This does not affect the strength of the hip at all. Not all these events are experienced by every patient but if they happen to you they are part of the normal recovery from the operation.
- A void crossing your legs.
- You should not move your leg across your body past its midline i.e. the line that divides one side of your body from the other through your belly button.
- lGet in and out of bed preferably leading with your operated leg. You can still get in and out of bed on the other side once your leg does not cross the midline.
- A void bending your hips past 90 degrees (i.e. an L shape between your upper body and legs).
When sitting down on a chair or toilet seat have your knee lower than your hip.
- A void turning your operated leg inwards/outwards.
- lWhen standing or walking do not swivel on your operated leg.
- A void putting pillows under your knees.
- A void lifting the leg off the bed with the knee straight.