Professor Brian Devitt is an internationally trained orthopaedic surgeon with subspecialty expertise in knee and hip surgery. He has a particular interest in sporting injuries including anterior cruciate ligament (ACL) reconstruction, meniscal repair, cartilage restoration procedures, multi-ligamentous knee reconstruction and hamstring repair. In addition, he cares for patients with degenerative conditions, such as knee arthritis, and performs partial and total knee replacements and total hip replacements.
Professor Brian Devitt is an internationally trained orthopaedic surgeon with subspecialty expertise in knee and hip surgery. He has a particular interest in sporting injuries including anterior cruciate ligament (ACL) reconstruction, meniscal repair, cartilage restoration procedures, multi-ligamentous knee reconstruction and hamstring repair. In addition, he cares for patients with degenerative conditions, such as knee arthritis, and performs partial and total knee replacements and total hip replacements.
Good evening, my name is Brian Devitt, I’m speaking this evening about ski related knee injuries. It’s a great pleasure to be able to join you again. So, I just want to share a quote which I heard from one of my mentors when I started off my fellowship in Vail, this quote stated, “If you’re to design a device to rupture an ACL you couldn’t get much better than a ski.” This relates to the fact that with skiing your knees are very vulnerable to turns because you’ve got a long lever which is the ski and you have your ankles held in position on your skis. So, Dr. Richard Steedman was one of the forefathers of sports orthopaedics and he worked in Vale, Colorado which is a good place for ski injuries because it was at the foot of a ski mountain.
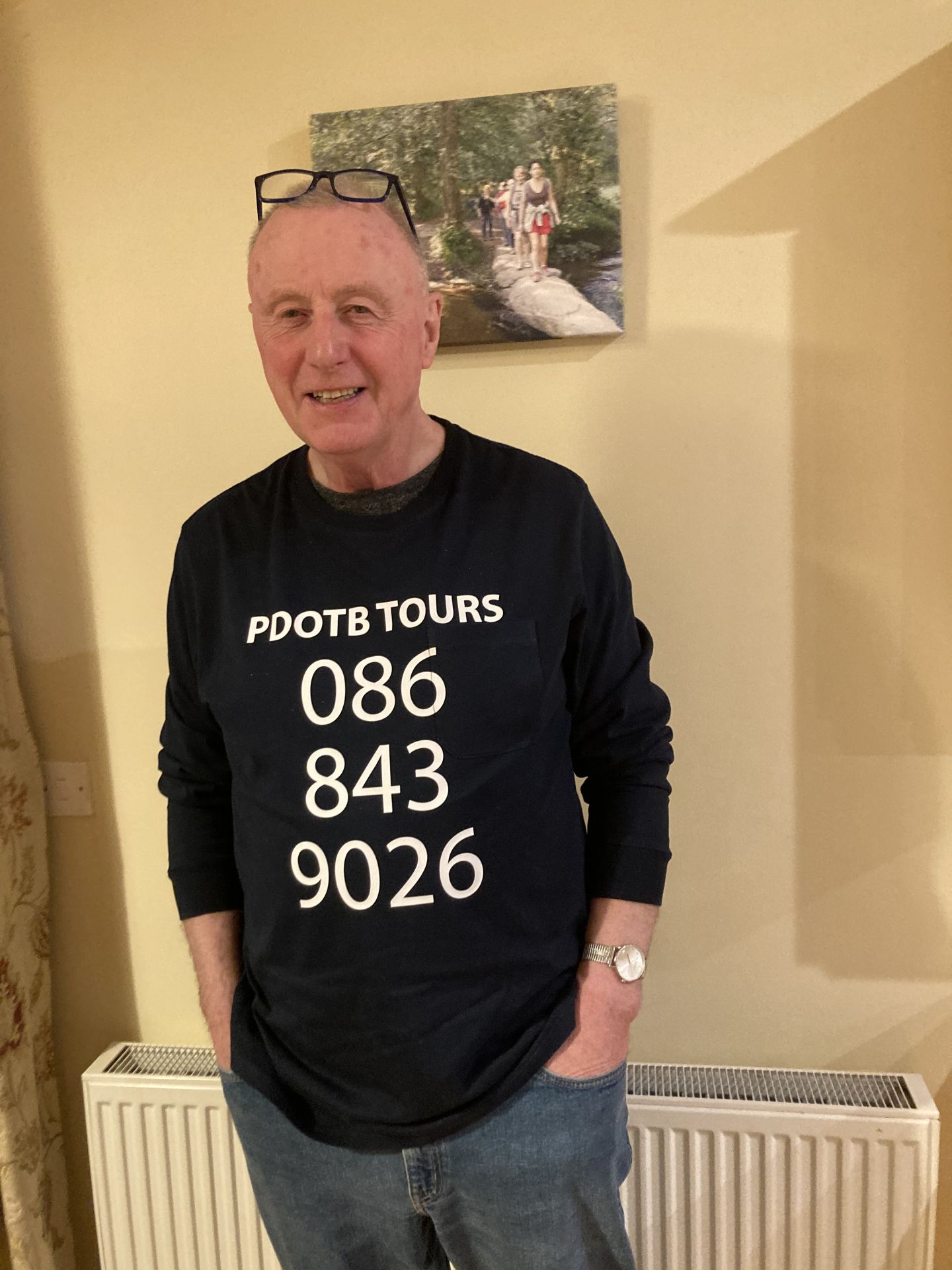
I like this particular picture which one of my colleagues sent me and perhaps we should all wear these when we’re starting off, but really ski slopes are the conveyor belt of knee injuries and other injuries which we will deal with in this series of talks. They are so because it has become hugely popular, back in the day it was skiing was for only the mega wealthy but nowadays most people go on a ski holiday or have access to it and they’ve become hugely popular.
They are risky sports’; in this little schematic we see that skiing has great preponderance of knee injuries whereas snowboarding you can get more kind of upper limb wrist related injuries. It’s just due to where the board is attached to the legs and but also the single board with the snowboard is less risky than the isolated skis on each limb.
In terms of the equipment, the equipment has changed remarkably and changes year on year in fact. But back in the day, you can see these guys no helmets, essentially the planks were lashed to the ankles and there was very primitive kind of footwear. But nowadays we have much more sophisticated equipment, you’ll see the boots have got these bindings which hold your foot in this flex position and the ski boots are then bound to the skis. This is one of the critical things is that when we’re starting off the ski, what we really need is a very loose or a loose enough binding so that if you fall over that your boot comes away from the ski and you don’t use your ski as a lever because that’s where you get a lot of knee injuries.
So, a lot of people come to the ski rental place and they’re very full of bravado from the previous year and they say that I’m an expert skier now because I’ve skied for one week. But what happens is the ski technician is tightening what we call the din on your bindings to make it more difficult for your boot to come away from the ski and as a result you’re more prone to knee injuries. So, if I were to offer any advice, I would say go low on the din or just be truthful about your level of expertise because that’s how the binding is set.
We also know that the skis have changed quite a bit and the skis are essentially making it easier for us to ski, you don’t have to lift your foot as much and it’s a lot about how your weight is distributed, but they’ve really improved safety. The terrain and conditions are really important. So, this is an example of you know very deep snow where you have to lean back on your skis but also and the opposite is true when you have very icy snow you have to lean forward more. So really the terrain conditions really determine how frequently people are injured and often when people aren’t familiar with different conditions that’s when they have greater chance of getting injured. So, if you’re not familiar with the terrain or how to ski in a particular terrain, it’s probably best that you speak to an expert or have some lessons. And also, be cautious when you’re finishing a run of the day is when you go down the blue slopes or the green slopes when there’s lots of people around, that’s where you can really run the risk of getting injured because it’s the traffic, but also the snow is very slushy and tends to be more sticky and that’s where people may get injured.
So, this is probably an example of what the ski conditions are like this year, and you have to be cautious where there’s exposed rocks or um where you’ve got grass exposed because it can stop the ski sliding. So, in terms of the mechanism of injuries, previously when I’ve done this talk, I’ve done a diagram, but I thought it was easier to show this video. You see a guy skiing at pace down the mountain and that snap you hear is not the snap of his ski releasing, but the snap of his ACL. So, you watch the person, he’s in deep slow, leaning, leaning back, back, back, back, and his knee is not in control and it’s his lower ski there those twists, and he twists on that knee, and he’s ruptured his right ACL in in this setting. So, if you have friends like those who needs enemies, it’s laughing at his buddy. But you can see very slowly he’s leaning back, back, back, immediately. He’s really put a lot of stress on his medial ligament. And this is the classic injury pattern we see with knee injuries.
But we can’t legislate for stupidity, this is another source of frequent knee injuries as well is that people just getting a bit carried away, maybe a few schnaps at lunch or a bit more of the red wine, that doesn’t really compute with the cerebellum when you’re skiing.
So, in terms of how do we manage on the mountain? Well, first of all, we do no harm. That’s the tenet of orthopaedics and medicine in general. I always use the phrase stay in your lane. And they put up these signs for a reason because they don’t want people to ski beyond their limits. It’s not so much at the start where it looks nice and flat, but it’s somewhere down the slope where you can really get yourself into a bit of trouble. So, I’d recommend when you’re starting off that you get lessons and you stay in your lane and go with a guide if you’re unfamiliar with the mountain.
Other things can be hazardous, it’s the people around us, it’s the fact that there’s alcohol being consumed and you’ve got people who don’t really have any regard for those around you and I think that’s very important just be aware that it can be a dangerous sport and you just have to be a little bit cautious.
I would suggest return to your comfort zone. So particularly when you’re starting off on the first day we used to have a phrase in our family you get your ski legs, and you really need to just to go up and do something gentle to begin with and not start off on a black or double black diamond unless you’re very familiar with the with the activity.
So, how do we manage then in the clinic? Well, in the clinic is where the dust has settled and that’s really where we have the opportunity to make a very safe and informed decision as to how to manage the patient. It’s the same way we manage any ski injury. But the recommendation I’d give to people is if you are injured on the mountain, what you need to do is get a diagnosis. So, you go down to the local medical tent, very experienced people, they’ll probably do an X-ray or maybe if they have access to an MRI and they’ll take a history of what the injury is. If you hear a pop and your knee twists and you’ve got a swollen knee well the chances are you’ve had an ACL injury to begin with so it’s very important that a thorough history is taken.
In terms of doing a history we just need to take our time and get the right history but if you have that pop and swelling that’s you know effectively, you’re an ACL injury until proven otherwise. The clinical examination is key and afterwards you’ll see the example that when you take your salopettes off, you’ll see a big swollen knee well that’s a bad sign unfortunately. So, the chances are you may have had you know an intraarticular injury which is an ACL rupture or maybe a ligament rupture. So, if that happens you really need to think seriously about getting that assessed.
In terms of management, we have to look at both sides as well and just to isolate one limb you’re going to miss the other side which gives a good example of normal. So be sure that if you’re being examined by someone that they expose both legs properly to have a good look and if you’re they’re not doing that, you probably need to get a different assessment. They typically would do X-rays, X-rays can be somewhat helpful, if you have this little flake of bone here that can diagnose an ACL, but some people use ultrasound, but it nothing compared to an MRI scan at the end of the day for diagnosing ACL injuries. But sometimes be cautious about what the quality of the MRI scan. If you’re shipping up a magnet to through to through the mountain, they’re not going to always have the premium MRIs up in the mountain so sometimes it’s best just to go down to a bigger city or town and have a proper diagnosis or come home and have a diagnosis. We’ve got very good scanners here and you can get it done very easily.
In terms of the next step, then it’s really referral. So, when you get home, if you’re injured, you really need to see an orthopaedic surgeon quickly. We’re very happy to facilitate people who haven’t got scans. We can get scans the same day and then we’re dealing with the issue in the cold light of day. So early diagnosis is much better than early treatment necessary and if the treatment is not appropriate and one of the things we really need to do is we need to make sure that someone is appropriately managed.
A lot of times if people are away, we there’s this pressure to get treated early and really there’s no urgency unless there’s a neurovascular injury to the leg the blood flow is being interrupted or very serious knee dislocation to treat this urgently. Most of these can be treated down the line. So, it’s important just to be calm about this and just get home appropriately and be treated.
In terms of non-operative versus operative intervention, well that’s the first thing we look at is can we avoid surgery in a lot of situations, and I give an example in the cases below where surgery is not always indicated. We want to remove the splints as soon as possible, a lot of people are put into splints, and you know I will be honest in that the medical companies over there they make money from splints. So, you get €200/300 cost for a splint but often times they’re not necessary. Now, if you have a medial ligament injury, a splint may be helpful for pain relief, but really, we need to get those knees moving. So, we try to take the splints off as soon as we can.
You never go into surgery with a person who doesn’t have a full range of motion. So, range of motion is really critical prior to any surgical intervention. We also want to get people weight bearing is tolerated and we get them using crutches. They often have a series of fancy crutches when we see people in this time of the year. But really, we want people to weight bear once they’re able to do so because that’s good for the cartilage. It’s good for restoring their normal biomechanics of their knee and great for the range of motion.
So, I’m going to go through a few little common scenarios. These are several cases which I frequently see at this time of the year. So, CASE ONE is a novice snowboarder. So, I get a letter 14-year-old snowboarder injury a week ago swelling within 12 hours. So immediately I’m thinking this guy’s got a serious injury. He had a plain film which was unremarkable except for that swelling in the knee. An MRI is performed which revealed a small medial condyle fracture and a grade two MCL sprain. So, the MRI will give you a grade but really, we want to examine this person in her own get the knee in her own hands so we can assess it. So, it’s a very common injury they talk about an ACL sprain in the image.
So, in terms of the history, so contact injury turning, didn’t hear a pop. So immediately I’m not thinking ACL here, fell to the ground, couldn’t wait bear, removed from the hill. That’s often a real factor; someone has to be taken off the mountain by the snow patrol. No immediate swelling, that’s good, but that letter did say swelling within 12 hours. Holding the knee in a flex attitude, well, that’s a position of comfort so if you any swelling in your knee, you’re going to hold it in a flex position. Walking with an antalgic gait, so that’s like a limp, mild swelling within the knee 10 to 135 degrees of flexion so that’s holding that knee in a flex position and the grade one injury in terms of my hands it’s differs to the MRI and the Lachman which is assessment of the ACL was negative so these are all good signs.
These are the x-rays so you can see it’s a 14-year-old, the grow plates these are the lines here they’re still open, but no suggestion of any serious ligamentous injury based on any little fragments of bone so that’s a good sign. This is the MRI scan, this is a one-shot MRI and we see over this side of the knee, you’ve got whiteness and that indicates some fluid. But this is a minor grade ACL or medial ligament and this beautiful structure in the middle of the knee, that’s the ACL. I spend most of my life dealing with that and that’s a really nice intact ribbon-like ACL, so that’s normal. So, in this person, you don’t have to do anything. Just get them moving, take them out of the brace and get them going. really focus on getting that knee extension going which is which is fantastic.
So, this is another case, a more serious case and this is a 42-year-old female. So recreational skier had an injury to the right knee following the fall. Unsure of the mechanism but just had a bit of a blur. She felt that both knees kind of went to the side, the ski bindings didn’t release and that was probably what put all the stress through the medial ligament but also the ACL, difficulty weightbearing afterwards, immediate pain and difficulty getting off the mountain with gross swelling in the right knee. So, in terms of the clinical assessment, difficult to stand. So, you know someone’s got a serious injury. On this side when I examined her knee that she had what we call grade three medial ligament laxity and grade three lachman test. So, the knee was very unstable in this situation and what we call ecchymosis or bruising on the inside of the knee. So really had a very loose knee and that was a more significant injury. So that’s one we recognise we’re going to need to treat and probably treat rapidly.
So, this is just the image from the side. So, I’ll draw your attention to the inside of the knee here. And you’ve got lots of whiteness which is fluid and blood and I’m looking for a black structure but it’s all this grey structure here. So, there’s very little in the way of her medial ligament intact which is unfortunate for her but does correspond with what I’m able to assess clinically is that this knee is really at a very serious injury.
I’ll then show you the image from the side. So, what we’re looking at on this image is we start from the outside of the knee, we see there’s lots of fluid here which is the white stuff on the outside. As we go into the knee, we see this black structure which lies between the two bones. That’s the meniscus or shock absorber. She does have a small tear to that. And then we see the middle of the knee, the ACL. So, you can see the absence of a nice ribbon-like ACL. The posterior crucial ligaments intact and the medial meniscus intact but then we see lots of fluid on the inside where she’s injured her medial ligament. So, this is a serious injury in an individual. So, this is one we don’t hang around with that we recognize we need to fix this.
So, these are just some findings from inside the surgery where you can look in the knee and this is what we see, and this is the big gap on the inside of the knee. So this is where the inside ligament has been injured and this is the structure inside the knee. This is where the ACL is torn so I’m able to reconstruct that. This is the end of the ACL, and the outside ligament of the outside had a small tear which was able to repair as well, and you see that there and then I’ll show you the picture of the ACL. This all went very well, but it was appropriate just to get this done at a timely manner. This little screw, we hold the ACL, this our lovely ACL in position here and the knee can get fully straight. This is an example of a more severe injury, and this is what we see on X-ray afterwards. So, the ACL is held in place with two screws. I repaired the medial ligament as well at the time.
So then we’re going to talk about people who present with more kind of chronic injuries. This is a guy came to me in what he called his bandy legs, so, he two what we call various knees, so he’s bow-legged. He’s a 62-year-old male, fanatical skier, skis couple of times every year, had a mechanism injury where he was twisting his knee getting out of the ski boot. So, not a classic kind of dynamic injury, more of a kind of a slower kind of injury with just a twist. He was able to ski and he said it settled after a few winds but did have a bit of swelling afterwards.
So, we see in the knee here, this is the X-ray, which the right leg shows there’s nice space between the two joints here, but on the left knee, there’s very little space and that indicates that this person has arthritis and the injury was just an exacerbation of their arthritis. So effectively what we need to do with this person is do what we call a partial knee replacement. So, the partial knee allows us to replace the arthritis on just one side of the joint which allows that person to get back to good activity very quickly afterwards and it restores the normal biomechanics of the knee without having to remove any of the ligaments which is excellent. So, this person was back skiing the following season h and it did very well.
The next thing I just want to talk about is joint replacement in the setting of skiing. Oftentimes people feel that their skiing days are over if they require a joint replacement and that’s not the case. In fact, one of the American athletes in her 40’s just won the World Cup Slalom Downhill skiing with the partial knee replacement. So, it’s certainly possible.
In terms of this person, a 65 year-old male, recreational skier, he refers as the best family holiday, the time when his teenage children will actually go on holiday with them because he’s footing the bill. In terms of what he was presenting with was progressive pain in his hips, struggled rotating his hip to get his boots on, pain at night, he felt he was waddling particularly difficult going up and down hills and wearing ski boots was uncomfortable and unstable for him. So, this is an example of his x-rays. So, these are both hips. So, you can see on the right side it’s a ball and socket joint with very little clearance between the ball and the socket. The left is a little bit better but still features of arthritis with extra bone here at the femoral head and femoral neck. So, this person had severe arthritis at both hips. He said he didn’t want the downtime of having one hip sequentially after the other. So, we did both hips, and he was very active very quickly back driving after three to four weeks and he was back playing golf after six weeks and was back skiing the following season. So, there’s no restriction in my mind for someone who wants to go back after knee or hip replacement. You must be a little bit cautious in terms of your level of skiing, you don’t want to go down something if you haven’t done it before. So just ski within your level.
Okay, so that’s it. That just gives you a bit of insight into what I deal with ski related injuries. But skiing is a great activity, it’s great for one’s mental health, it’s great fun and I was just teasing people that the muscles that will hurt the most are your stomach muscles from laughing so much. If you do get injured just be cautious, get home as quickly as you can, make a diagnosis, and we’re very happy to deal with you and get you back on the slopes hopefully. All right, thank you very much.
I think the fastest way to diagnose is to take a history, as I mentioned it’s a really you get a very good indication of what someone has done based on just taking the time to speak to them. Most people tend to rely on radiology a lot, but it has limitations and it doesn’t allow us to assess laxity or what we can determine with our hands, but MRIs have really revolutionised how we do diagnose knee injuries. So, it is certainly part of the package. In terms of urgency requests that I know the GP liaison service within Sports Surgery Clinic is very helpful that patients can ring and to see if it’s appropriate that some of the injuries go to our clinics. Obviously, we don’t deal with you know urgent fractures or trauma, but we deal with most other specialties including foot and ankle, shoulder and obviously knee and hip. So, the GP liaison service will put the individual in touch with the right teams and will get them seen very quickly to just take the stress out of the situation. Our practice that we have a lot of clinical specialists are around all the time. So, the person may not get to speak to me directly, but our PAs will put them in touch with a clinical specialist, and we can also organise scans very quickly through the hospital so that we know we’re getting high quality.
Yes. So, this particularly for the likes of ACL which I’ll take an example. So, it all depends on the severity of the injury. Some situations like I mentioned in my talk need to be done urgently because someone’s knee is so unstable or very lax. But the likes of ACL surgery, we are much rather a leg that’s happy and that’s able to move, that’s important for a good outcome after surgery. So, there’s no huge advantage to doing surgery early doors and sometimes there’s a disadvantage that you get more stiffness. So really, we make a determination on that based on how the knee appears to us when we assess it.