Watch this video of Professor Brian M Devitt, Consultant Orthopaedic Surgeon specialising in the Knee, Presenting on ‘Summer & the living is easy! Staying on track with Knee Arthritis’.
This video was recorded as part of UPMC SSC’s Online Public Information Meeting, focusing on ‘An Evening for Hikers/Walkers’.

Brian Devitt is an internationally trained orthopaedic surgeon with subspecialty expertise in knee surgery. He is particularly interested in sporting injuries, including anterior cruciate ligament (ACL) reconstruction, meniscal repair, cartilage restoration procedures, multi-ligamentous knee reconstruction and hamstring repair. In addition, he cares for patients with degenerative conditions, such as knee arthritis, and performs partial and total knee replacements and osteotomies.
Brian completed his medical school training at University College Dublin, Ireland, and carried out his specialist training in Trauma & Orthopaedics at the Royal College of Surgeons in Ireland. He also achieved a Masters in Sports and Exercise Medicine. Brian pursued a career in academic orthopaedic sports surgery and completed three years of fellowship training. The first year was a research fellowship at the Steadman Philippon Research Institute. He then completed a clinical fellowship in sports surgery at the University of Toronto. Finally, he completed two clinical fellowships in Melbourne; the first was a knee reconstruction fellowship at OrthoSport Victoria (OSV) and the second at Hip Arthroscopy Australia. Following his fellowship, Brian worked as a consultant orthopaedic surgeon at OSV and Epworth Healthcare.
Brian has a keen research interest and is a Full Professor and Chair of Orthopaedics and Surgical Biomechanics at Dublin City University. He has extensive research experience focusing on clinical outcomes and biomechanical studies. He has published widely and frequently speaks at national and international meetings.
Good evening. My name is Brian Devitt, I’m going to speak to you about staying on track with knee osteoarthritis, and this is with relevance to walking and hiking. I want to first off show you a picture of a former patient of mine. This is a lady who’s in her seventies, and she has embarked on a charity walk in Vietnam; she had previously had a total knee replacement eighteen months ago, so there are a few features I just want to point out first of all if she’s smiling! She’s doing very well following her knee replacement; secondly, she’s using a stick to help her get up what is a relatively steep slope; she’s wearing the appropriate shoe wear she doesn’t have too much to encumber her in her hike in terms of carrying a lot of load, and she’s willing to help or receive help from the tour guide who’s bringing us along so when in Vietnam we learned an awful lot of things but one of the most important things we learned to some of the quotes from Confucius who is a Chinese philosopher, and he told us it doesn’t matter how slow you go as long as you don’t stop I think this is hugely relevant when it comes to the management of knee arthritis but also activity in the setting of arthritis it’s really important that we keep on going.
We all come in different shapes and sizes, and it’s the same with respect to our needs. We look here on the left side of the screen we see what a normal alignment, just two straight legs is; we see various alignments of what we know as bow-legged and common pylons, and we also see knock knees or valgus alignment where on the right-hand side of the screen now all the people who come in this in these different shapes normally but when it comes to pathology we also see people develop these shapes of their knees as time goes on and this is quite relevant in terms of how the ways when we walk goes through our knees when we’re in a neutral position the weight goes directly in the middle of the knee which is equally shared in this bow leg position the way it goes on the inside of the knee and in this knock knee position the weight goes on the outside of the knee so this has an impact in terms of how we progress with wear and tear as Life Goes On.
I’m going to show you a few picture examples or X-ray examples, and one of the things we use as orthopaedic surgeons to diagnose arthritis it’s key to take the history from the patient as to where the pain is and when it occurs, but an x-ray is very helpful the most important thing about the x-rays the person is standing, and we can see on both legs here that there’s very little space on the inside of the joint both of the right leg and of the left leg and we refer to this as decreased joint space or also what is known as bone on bone osteoarthritis so this happens in a situation where someone has bowed legs we also look at the kneecap, and that’s really important when it comes to walking because as you walk down the hills or down stairs or even upstairs it puts a huge amount of stress through your kneecap so it’s really important that we would look at this and this kneecap is not too bad it’s got a little bit of decreased space, but there’s plenty of life left in that yet.
We often get patients referred to us with an MRI scan and MRIs will diagnose a lot of the soft tissue conditions but we can also see arthritis so I’m going to explain initially we’re looking at this MRI looking at your knee from the front so this here is your kneecap I’m going to work our way towards the back anything that shows up as white on these scans indicates fluid or increased stress within the bone I’m going to point that out as we go so we’ll work our way back through the MRI it’s a little bit shaky so excuse me and I’m looking at the fluid in these we know that this knee is not in a great state and we can see that the bone in this area on the inside of the knee is very white and that indicates that this bone is under a huge amount of stress and the reason it’s under stress and I’m going to go through that again is because the meniscus which is a shock absorber in the knee has been damaged so you see this black structure is the meniscus and you see it’s being put down to the side of the knee and underneath you’ve no cartilage on this inside of the knee and that’s why a lot of people come to us to think they have a meniscal tear but in fact the horse has long since bolted its arthritis is the situation so this is how we see it on an MRI and the previous x-ray that we saw where your bone and Bone arthritis is how we see it on an X-ray so we do use all of these modalities to diagnose the injury and the presence of arthritis .This is another x-ray which shows arthritis not on the inside of the knee like previously but on the outside you can see the shape of the leg is different from the normal leg which is nice and straight we see on the outside of the knee you have wear and tear here with extra bone forming here in this region here and you can see there’s bone and Bone arthritis on the outside of the knee we look at this example of the kneecap we see that there’s a lot of extra bone around the kneecap and no space between the front of the kneecap and the femur so this is an example of someone who has not only wear and tear on the outside of the knee but also wear and tear on the front of the knee so you imagine they’re going to have an awful lot of pain walking down stairs kneeling or any type of movement going from a seated to a standing position.
Now we’re going to have a little bit of physics to understand why we have pain in the knee when we have arthritis and we walk and physics so this is a pictorial example of Isaac Newton so Isaac Newton discovered gravity but he also discovered a lot of other important physics and equations and theories and one of the things that he recognised is that gravity is a huge part to play but also within the knee as we expect we extrapolate that to the load going through our knees when we walk it is very important so if we look of just walking the weight that goes through our knees each individually when we walk is twice our body weight when we walk downhill that increases to four times our body weight and if we were to run that can go up to as much as eight times our body weight so that’s why if someone might be fine while standing but when they walk the pain increases it’s because the load going through the knee also increases so let’s do a small little calculation so we’ll take a hundred kilogram male so that’s a big man may be carrying a bit of extra timber so 100 kilograms that person walks down here 400 kilograms goes to each individual knee with that action now if he was to lose a moderate amount of weight which is ten kilograms or ten percent of his body weight which would take a bit of effort he would find that forty kilograms less goes through each knee as he walks downhill so this is a very important to remember in terms of the loads that go through our knees when we walk and also as a means of treatment for arthritis it’s very important.
In terms of the injuries we get while walking, I’m going to give you a couple of examples of how to avoid injury, to begin with, so you don’t end up in my office at any time. So first of all, it is knowing your limits so when you start walking or if you’ve gone from a period of sedentary period to an active period, it’s important that you go gradually; you don’t go start hiking Mount Everest when you’re just starting you’re walking so it’s very important to know your limits I think that’s one of the things we saw after covet is when people were relatively sedentary they went out to walk every day of the week we saw people with a lot of issues developed quite quickly so if you’re starting to walk just start walking on the flat first and if you want to then engage in some steps that are appropriate if you have no pain or then walk up and down Hills as you see fit. it’s often best to be preconditioned so you want to improve your ankle strength and balance and nowadays we recognise that Pilates is really a great treatment for all types of ailments and it’s incredibly important with regard to improving your core strength but also the strength of your quadriceps and hamstrings and also your ankles if you’re particularly when you see reformer Pilates these can be very effective as an all-around holistic method to improve your strength and balance we recognise hugely as I saw in the picture at the start is that the use of hiking poles is really important particularly when you’re going up and down hills because it allows you to take the load off the front of the knee and share it with the load in your arms it also gives you an improved workout with your upper body so using more walking poles is actually very sensible when it comes to hiking so that’s something we would recommend very much so the use of appropriate Footwear so going hiking in a pair of sandals is not appropriate because you’ll end up rolling your ankle or you’ll load inappropriately particularly on uneven ground and that tends to put increased stress through your knees or a little needle there are some blisters that you’ll try to you’ll walk a bit more you walk differently and that puts increased load through your knees so that’s it and not a good wise thing to do is to wear inappropriate Footwear and we recognise wearing properly fitted Footwear with appropriate socks and trying to avoid getting the likes of blisters because they do change the your gait and it’s important that you try to maintain a normal gait that you equally distribute the weight throughout your knee and not in one certain area and then just common sense and hydrate adequately when you’re tired of fatigue you tend to stress our knees quite a bit more so just have an appropriately distant walk so you’re not very fatigued at the end of it or you’re walking in incorrectly which puts more stress to the front of your knees it’s really important that your general health is well maintained as well .
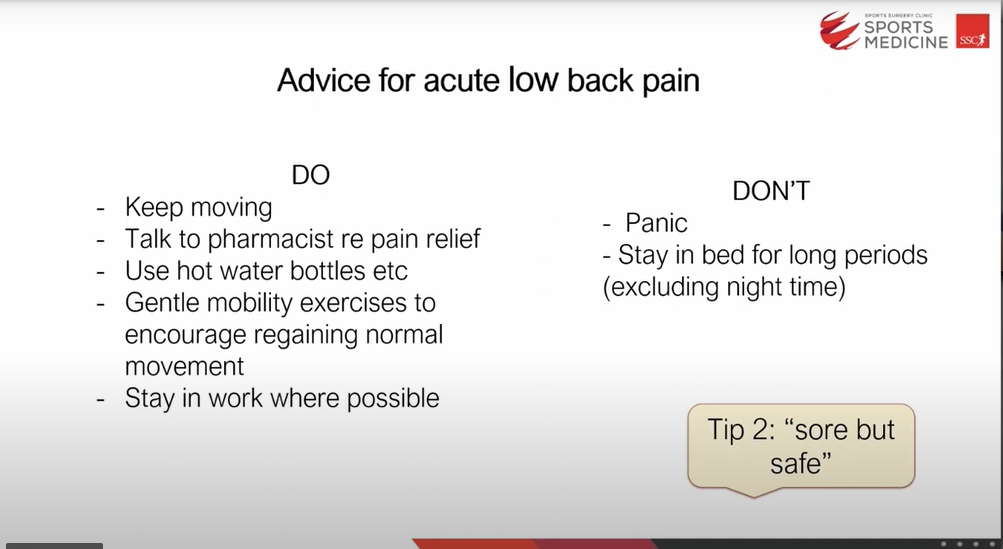
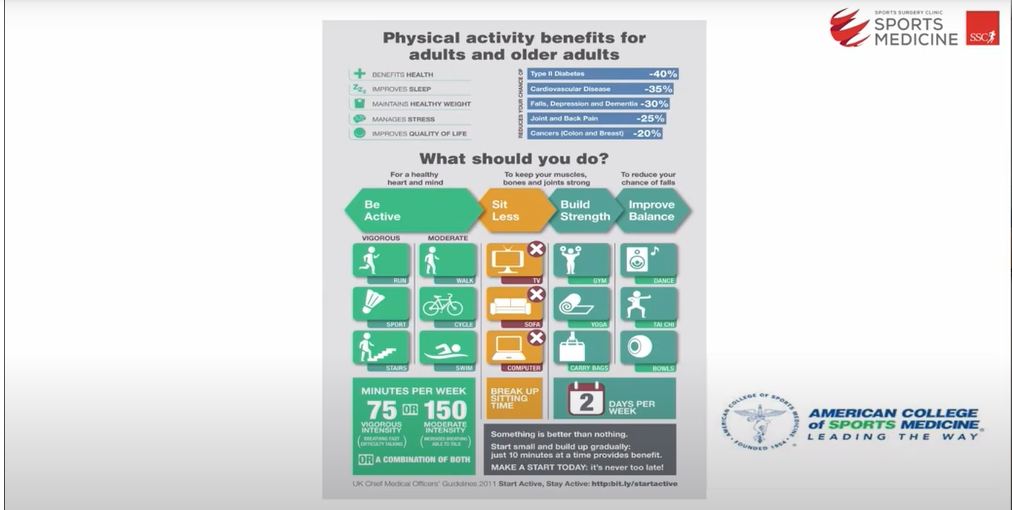
Let’s just look at arthritis unfortunately if you can’t avoid injuries and you do get some injuries or arthritis how do we manage them it’s really important that you understand this so I like this quote from Macbeth I’ve used it before in different talks where it says ‘ Eye of newt and toe of frog, Wool of bat and tongue of dog, Adder’s fork and blind-worm’s sting, Lizard’s leg and owlet’s wing, For a charm of powerful trouble, Like a hell-broth boil and bubble’ if we got the lighting to come on as well give it a bit more impact but this is a quote from Macbeth but none of these things work for osteoarthritis you can rest assured you don’t have to have any far-fangled poisons or potions to get you to improve your arthritis these things don’t work I oftentimes get patients coming into my room and they’ve consulted Dr Google and they come in and say well this laser work doctor and really I try to keep it very simple there’s a few tried and trusted things that work for arthritis and I would encourage you to follow the trial and trust it and not the far angle treatment so these are the treatments that do work so physical activity is important just like the lady who’s walking after a knee replaced and walking beforehand can be effective but we try to avoid heavy load activities that put more stress to our knees weight loss is really they’re probably one of the best treatments but it’s not an immediate treatment to lose weight so weight loss is very helpful as per Isaac Newton’s knowledge and equations earlier on acupuncture has not been shown to work massage can be helpful for tight muscles bracing can occasionally be helpful and maybe a compressive brace can give you a bit more feedback in your knee in Soles likewise have not been shown to be hugely helpful but they do make footwear fit more appropriately and glucosamine has not been shown to be extremely helpful but it doesn’t do much harm and it’s cheap so I wouldn’t be overly against the use of glucosamine as an oral tablet.
We then look at pharmacological treatment and we recognise that anti-inflammatories do work so if you have swelling in your knee it shuts down your muscles so if we can get rid of that swelling it allows your knee to function much better a steroid injection and can be helpful particularly if you have swelling but it’s not it’s not a long lasting effect it just has a short-term effect the use of hyaluronic acid in this recommendation and that’s from the American Academy of orthopaedic surgery has not been shown to be effective it may be more effective in younger patients but not in patients with Bone arthritis and then plated rich plasma can be helped in some circumstances but it’s not the go-to in every case and then we look at surgeries and what stuff that we do as a surgeon so washing the joint out with the camera that is not effective it used to be an old-fashioned treatment but we don’t do that anymore sometimes if people even in the setting arthritis have a flipped piece of soft tissue like meniscus remove that can give them and some temporary relief but it doesn’t remove the arthritis it just removes the soft tissue which might be impinging or getting in the way, doing an osteotomy which means cutting the bone and changing the shape of the leg can be helpful in certain cases and then a joint replacement has been shown to be very effective in the right setting at the right time so, one of the take-home messages I always say to patients is your objective is to avoid people like me as long as you can.
When your arthritis gets quite severe we are very helpful in terms of believing that pain and getting you back on track so the effective method just to reiterate our weight loss modify your activity if you’re doing things that are hurting you a lot like walking down stairs or and you know walking down slopes then I try to avoid that as best you can and it’s also important to maintain the strength of your of your muscles and do so in a manner that doesn’t hurt you so much so doing the likes of cycling swimming if you have advanced arthritis can be very good to maintain your motion the use of anti-inflammatory medication is very important there’s a limited role for arthroscopy and knee replacement when ready and when I tell patients they know they’re ready when they pain at night or pain at rest that really affects the quality of life and that’s where it’s really important so I’m just going to give an example of this is a knee replacement so this is one of the ladies earlier on who had the wear and tear to the outside of the joint and the front of the knee and this is what we did we gave her a knee replacement and this lady was back walking and hiking and it’s not quite the picture of the woman I saw at the front but very similar back to a very active quality of life we see how straight we get the leg afterwards and this is replacing the kneecaps that was extremely badly worn with a resurfacing of that kneecap or patella as we talk about so allowed her to walk downstairs without any major problems we also sometimes just replace one part of the joint so on this right leg here we see the inside part of the joint has arthritis and decreased joint space and extra bone here and in this case we just replaced this side because the rest of the side was relatively well maintained and allows patients to get back to a very good level of function very quickly after surgery so patients often ask me how active can I be with a knee replacement and I often remember a patient of mine who is a farmer from an area in Victoria when he’s working Australia called Gippsland and I remember this patient came in and he came at six months following surgery and he asked him that his knee hurt and he said occasionally it hurt I said when does it hurt he said well after shearing 50 sheep it became a little bit painful and he told me a very good quote which I often tell patients when I see them in the clinic and what this said he said was I quickly realised that it was a case of my knee getting used to me and not me getting used to my knee so this is a real paradigm shift in my mind in that when you have a knee replacement just go off and do what you want to do if you Molly coddle that knee and if you don’t move it you’ll be storing sore and stiff you could off and do what you want to do whether it’s um cycling whether it’s playing tennis whether it’s surfing whether it’s shearing sheep just do what you want to do and your knee will follow suit so I’m very happy to take some questions later on and I hope you get back on track with knee arthritis .
Well, it’s quite common to guess growing pain while walking. I suppose it depends on the patient’s age, but typically if someone has pain, it’s either a muscular injury or strain or can relate to arthritis. It’s a very common site to get arthritis within the groin, and it’s typically a pain that comes on after exercise as it gets more severe. You can get it at rest or at night, and that’s when you really should have something done about it.
Yeah, a walking stick can be very helpful. Essentially it’s typically used in the opposite hand and essentially offloads some of the weight going through the hip, and the muscles that are attached to the side of your hip really undergo quite a bit of stress when you have arthritis because the joint is irritable and this is an ability to offload that by using the walking stick around the opposite hand typically.
Yeah, for the same reason walking forwards are an excellent idea, and people tend to use two poles nowadays. I know the picture I showed at the start of my talk was just the solitary pole, but she used two poles. I think they refer to it as Nordic walking, and where they use two folds is great because you’re able to particularly going uphill but also going downhill, you’re able to take some of the load off the front of the knee, so you use your arms to push you up and keep the stick and quite vertical, and it allows you to exercise your upper body but also offload the knee and takes a lot of the stress off the front of the knee and makes it somewhat easier
Well, as I referred to with Isaac Newton and the importance of gravity and weight are hugely important in terms of the load going through a joint, so, not just your knee joint but all your joints of your body, so if you’re carrying excess weight, you will put a significant amount of weight multiple times your weight through that joint and in terms of excess ways and inflammation I think the excess load is going to give rise to further inflammation within your joint, and I know there are further studies that probably have looked at obesity and inflammation in general but specifically with the joint it’s very much the load that goes through the joint causes the irritability.
The new support can be helpful in certain circumstances. I think you know you can go from very fancy braces, which offload one particular compartment of the knee and they can be somewhat awkward to wear but can be effective, to a simple sleeve which essentially can give some feedback or what we call proprioception is where you know knowing where your joint is in space and sometimes you have swelling in the knee using a compression sleeve is very effective and but there is no proven evidence that they’re going to reduce the progression of arthritis they just make you feel a bit better during exercise sometimes.
I just think we’re not there yet. I think, realistically, stem cells offer a great possibility, perhaps in terms of the management of arthritis, but we really don’t have the answers yet. I follow the research quite closely on this issue, and really we don’t have the evidence to support the use of stem cells. One of the things which are very interesting is some of the guidelines from Australia, where I worked previously; they said you shouldn’t really be involved or go to someone who is delivering stem cells without it being involved in a randomised control trial, and you’ll find that most of the people who supply stem cells are doing so too for a commercial gain it’s not based on research or evidence so I would say beware in those circumstances because you can find yourself out of pocket a lot without any proven evidence it works.